 中央研究院 生物化學研究所
中央研究院 生物化學研究所
BACKGROUND. Inadequate tuberculosis (TB) diagnostics are a major hurdle in the reduction of disease burden, and accurate point-of-care tests (POCTs) are urgently needed. We assessed the diagnostic accuracy of Fujifilm SILVAMP TB lipoarabinomannan (FujiLAM) POCT for TB diagnosis in HIV-negative outpatients and compared it with Alere Determine TB LAM Ag (AlereLAM) POCT and a laboratory-based ultrasensitive electrochemiluminescence LAM research assay (EclLAM).
METHODS. In this multicenter diagnostic test accuracy study, we recruited HIV-negative adults with symptoms suggestive of pulmonary TB presenting to outpatient health care centers in Peru and South Africa. Urine samples were tested using FujiLAM, AlereLAM, and EclLAM, and the diagnostic accuracy was assessed against a microbiological reference standard (MRS) and a composite reference standard.
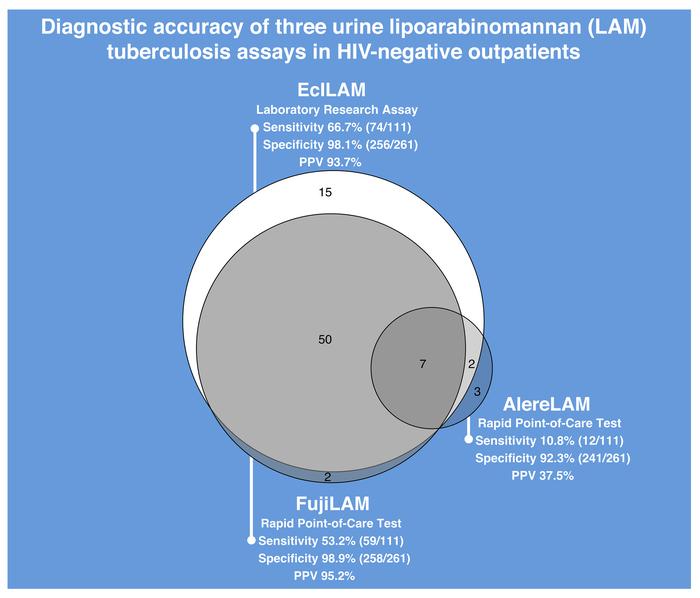
RESULTS. Three hundred seventy-two HIV-negative participants were included and the prevalence of microbiologically confirmed TB was 30%. Compared with the MRS, the sensitivities of AlereLAM, FujiLAM, and EclLAM were 10.8% (95% confidence interval [CI] 6.3%–18.0%), 53.2% (95% CI 43.9%–62.1%), and 66.7% (95% CI 57.5%–74.7%), respectively. The specificities of AlereLAM, FujiLAM, and EclLAM were 92.3% (95% CI 88.5%–95.0%), 98.9% (95% CI 96.7%–99.6%), and 98.1% (95% CI 95.6%–99.2%), respectively. Positive likelihood ratios of AlereLAM, FujiLAM, and EclLAM were 1.4, 46.2, and 34.8, respectively, and positive predictive values were 37.5%, 95.2%, and 93.7%, respectively.
CONCLUSION. Compared with AlereLAM, FujiLAM detected 5 times more patients with TB in HIV-negative participants, had a high positive predictive value, and has the potential to improve rapid diagnosis of TB at the point-of-care. EclLAM demonstrated that additional sensitivity gains are possible, which highlights LAM’s potential as a biomarker. Additional research is required to assess FujiLAM’s performance in prospective cohorts, its cost-effectiveness, and its impact in real-world clinical settings.
FUNDING. Global Health Innovative Technology Fund, the UK Department for International Development, the Dutch Ministry of Foreign Affairs, the Bill and Melinda Gates Foundation, the Australian Department of Foreign Affairs and Trade, the German Federal Ministry of Education and Research through Kreditanstalt für Wiederaufbau, and the NIH and National Institute of Allergy and Infectious Diseases.